@A hypothetical pathogenesis model for androgenic alopecia clarifying the dihydrotestosterone paradox and rate-limiting recovery factor (English 2017)
2021-11-19 links: Hair Loss DHT
(English 2017) A hypothetical pathogenesis model for androgenic alopecia clarifying the dihydrotestosterone paradox and rate-limiting recovery factor #
- This guy has a literature review on botox for treating chronic galea tension, which does indeed improve hair count.
- General consensus: DHT binds to androgen receptors in dermal papilla cells and tissues surrounding the AGA-prone follicles. As it accumulates, the tissue becomes sensitive and miniaturizes.
- Treatment with Finasteride and so on is motly limited to stopping progression, 10% increase in density, and some thickening.
- Studies with identical twins have demonstrated that it has a genetic predispositon, but one twin can go bald significantly faster.
- Some other untersuchungen:
- Miniaturized follicles may suffer from a defect preventing conversion of stem cells to progenitor cells. Doesn’t say much about how it fails, though.
- Deterioration of the arrector pili muscle: once it reaches the point of detachment from a hair follicle unit (why? Doesn’t say apparently) hair loss may be permanent.
- Various molecules/cytokines/signaling proteins/etc (IL-1α, IL-1β, TNF-α) are observed alongide AGA and conditions concurrent with it. A relationship between them and androgens is not explained.
-
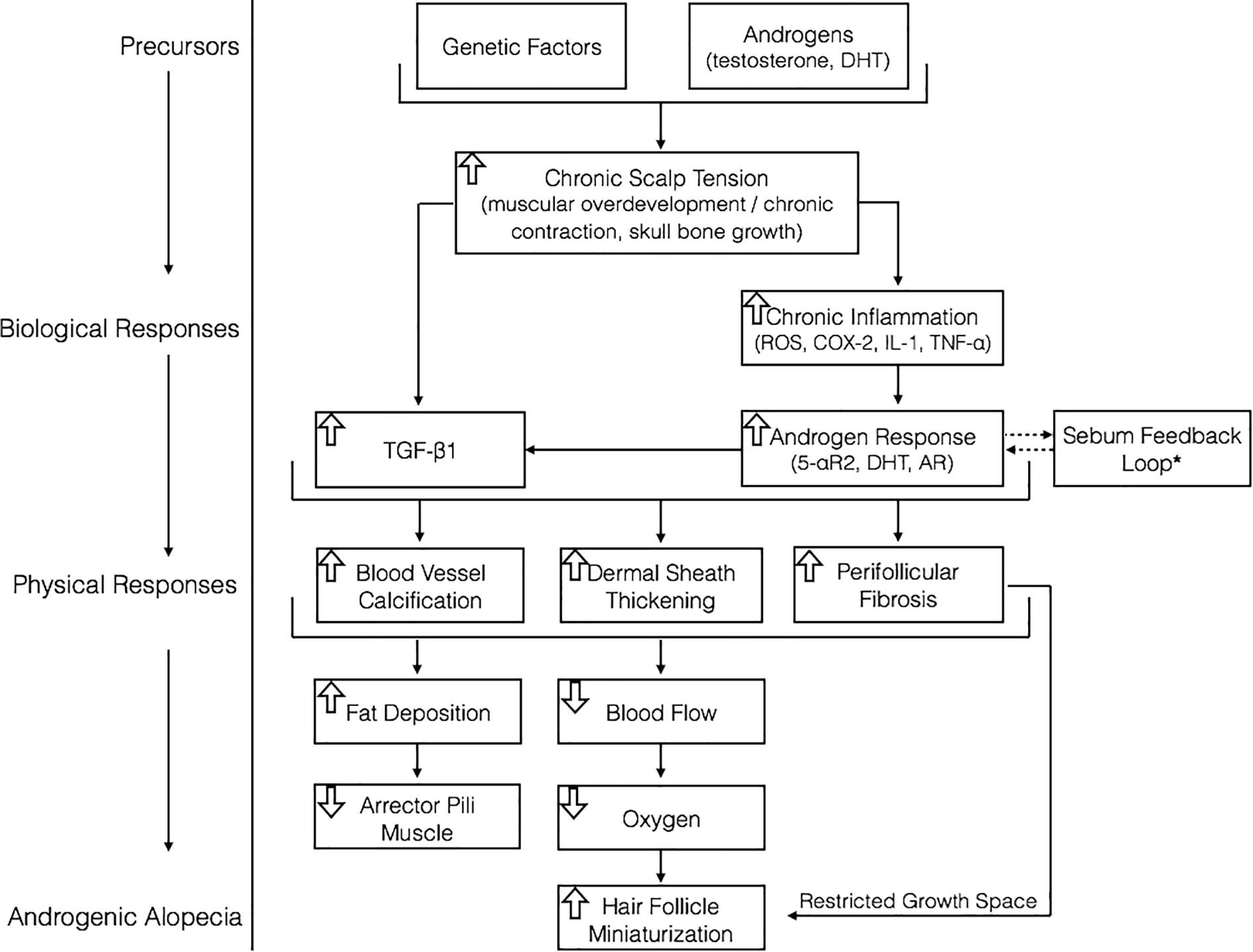
Hypothesis: Chronic scalp tension induces an inflammatory response in AA-prone tissues, DHT increases as part of the inflammatory response, but does not directly minaturize follicles, but is a co-mediator of tissue dermal sheath thickening, perifollicular fibrosis, and calicification.
-
Highest tension points correspond to the first places of onset. This stress may be influenced by androgens and alters the inactive standby of Androgen Receptor co-activator Hic-5/ARA55 and androgen-mediated TGF-β1. It’s tension->ARA55->TGF.
- TGF-β1 increases aortic calification in sheep, potentially as a result of alkaline phosphatase activity. Scalp dermal papilla cells produce higher levels of TGF-β2 than beard DP cels; TGF-β expression is higher in AGA cells than facial/body hair, it mediates calicifcation in both, but their differences in expressing TGF-β could explain why facial/body hair isn’t lost.
- Mechanical tension in periodontal tissues induces COX-2 expression and upregulates TGF-β.
- A relationship between skull shape and MPB, and androgen-mediated skull development, was postulated.
-
AGA progression coincides with APM (arrector pili; the muscles that make goose bumps) degeneration and its replacement with fat below vellus hair follicles.
- Not due to chronic unuse, but chronic tension: a study of toxin injections targeting the APM showed an increase in hair count.
-
AGA tissues express higher ROS activity, which increases TGF-β1, an androgen-mediated signaling protein expressed more highly in AGA-affected skin.
-
Elevated PGD2.
-
Enlarged sebaceous glands and higher sebum production in affected hair follicles!
-
Microorganisms? “One study observed porphyrins in 58% of pilosebaceous canals in those with AGA versus 12% in non-AGA controls.”
-
A study showed that 37% of those with AGA have significant inflammation+fibrosis surrounding thinning follicles - perifollicular fibrosis.
- Increased collagen deposition below AGA miniaturizing follicles, 2 to 2.5-fold enlargement of follicle dermal sheath made up of dense collagen bundles.
- Balding vertex/temples regions have near 4-fold increase in collagen fibers. The progression of this fibrosis may match/be concurrent with AGA as a whole.
- Scleroderma, an overproduction of collagen in cutaneous tissues: in the dermis/epidermis, leads to hair loss after scarring from an acute injury.
- The earliest signs of fibrosis in scleroderma patients appear in the areas of severest vascular parturbation.
- In liver fibrosis for instance, excessive extracellular matrix synthesis and deposition lead to microvascular/nutritive degradation - leading to decreased oxygen/nutrient supply. This could probably be extrapolated to AGA.
- Unlike aromatization, 5-AR is not oxygen-dependent.
- Fibrosis/calcification is commonly observed in heart disease, which is characterized by build-up of fats, calcium, cholesterols/plaque in arterial pathways. Early onset AGA might be a predictor for heart disease.
- CVD develops ~10 years earlier in males than females, and males have 2-3x higher calcium scores in coronary arteries.
- May impose physical restrictions to the maximum diameter of follicles.
-
Calcification of capillary networks supporting AGA-affected follicles.
- Transcutaneous oxygen in frontal scalp regions of AGA men is 60% of non-AGA counterparts, implying microvascular deficiency.